Key Takeaways
- Substance risk in music arises from touring stress, easy access, venue culture, myths about creativity, and a lack of awareness about safer coping strategies and early warning signs.
- Early signs include rising tolerance, using to play or sleep, missed rehearsals, and conflicts with bandmates.
- Outpatient and IOP keep artists working during structured care and can match inpatient outcomes for many.
- Choose programs that use evidence‑based therapies and FDA‑approved AUD medications, plus peer support that fits you.
- Severe withdrawal—hallucinations, confusion, seizures, or delirium tremens—requires immediate hospital detox for alcohol.
- Residential care helps when home is unsafe, triggers are intense, or constant medical monitoring is needed.
- Austin offers music‑friendly options, including programs that integrate therapy with music and flexible schedules for working artists.
- When reviewing alcohol treatment centers in Austin or any Austin rehab, confirm licensing, medications, and flexible schedules.
- “Luxury alcohol treatment” adds comfort and privacy; outcomes still depend more on clinical quality than amenities.
- Build aftercare with relapse‑prevention skills, community groups, and telehealth to stay engaged while touring.
- For local help, compare drug & alcohol rehab Austin programs for IOP availability, evening groups, and co‑occurring care.
- If you are in crisis, call 988 or go to the nearest emergency department.
Table of Contents
Austin has a deep music culture and a strong treatment community. This guide explains why substance use is common in the music world and outlines practical, outpatient paths in Austin—so artists can get help without stepping off the stage for good.
Why substance use is common in music
Working conditions and tour life
Culture, access, and pressure
Mental health and self‑medication
Signs an artist may need help
Early flags
Urgent red flags
Seek medical care immediately for alcohol withdrawal danger signs: confusion, hallucinations, severe agitation, seizures, or signs of delirium tremens. These symptoms require hospital detox for alcohol with close monitoring and medications.
Proven care—without leaving your life behind
What “outpatient” means for musicians
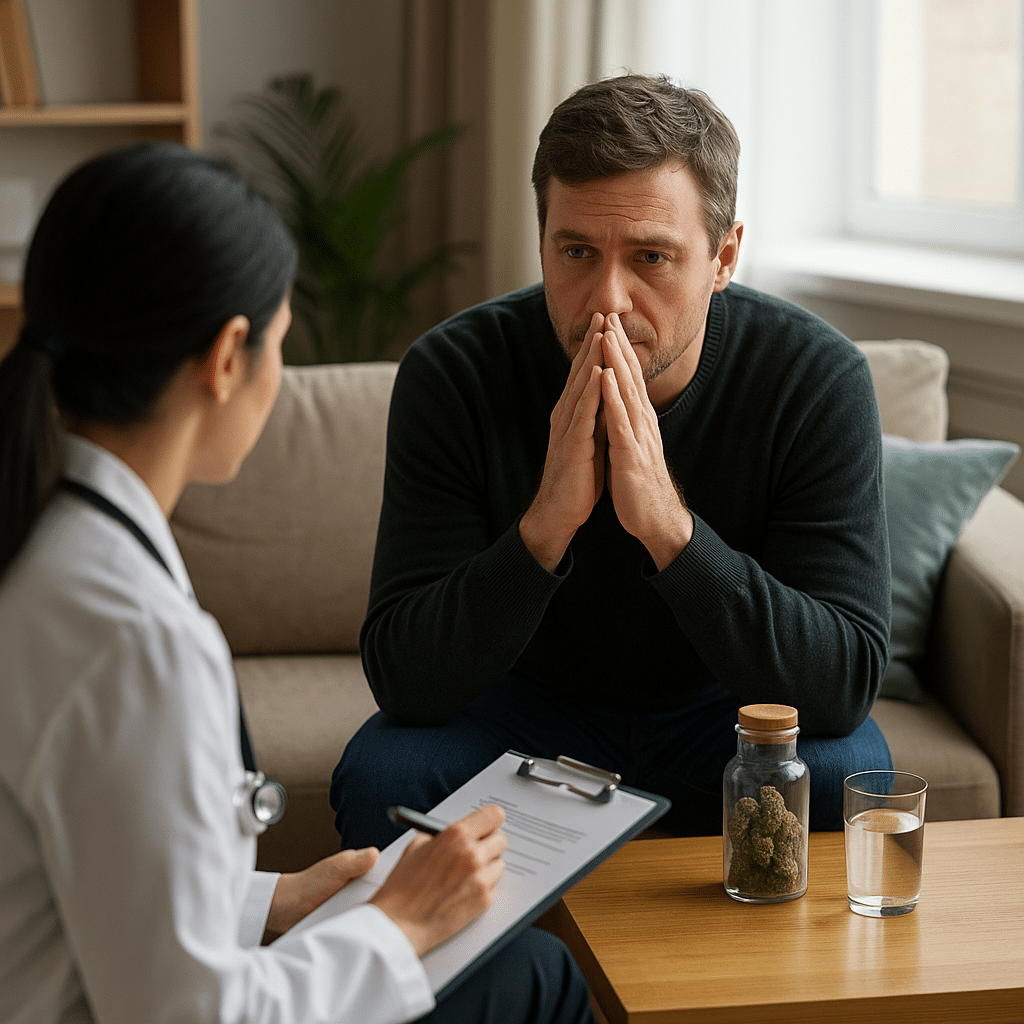
Outpatient and intensive outpatient programs (IOP) deliver several hours of treatment on set days each week. Many artists use IOP to keep gigs, studio work, or family duties while getting therapy, skills training, relapse‑prevention planning, and medication management when needed. Research shows IOPs are an important, effective part of care and, for many, work about as well as inpatient.
Evidence‑based tools that help
- Therapies: CBT, DBT skills, motivational approaches, family work.
- Medications for alcohol use disorder: naltrexone (oral or monthly injection), acamprosate, and disulfiram—paired with counseling.
- Peer support: AA or secular options such as SMART Recovery.
A personalized mix improves outcomes; there is no one “right” path for everyone.
When inpatient or residential is a better fit
Break Free from Addiction. Detox Safely in Austin Today.
Medically Supervised Detox – Compassionate Care Starts Here.
Austin options: outpatient care designed for working artists
Music‑assisted treatment in Austin
Austin has treatment options that integrate music into evidence‑based care and offers multiple levels: medical detox, residential, outpatient & intensive outpatient, PHP, medication‑assisted treatment, and telehealth. Facilities include comfortable living spaces and fully equipped music rooms, which can help artists engage in therapy without losing their creative identity.
Choosing an Austin rehab that fits a musician’s life
Look for licensed, alcohol treatment centers in Austin that provide:
- A full continuum (detox, residential, PHP, IOP, outpatient).
- Therapies with evidence behind them, plus access to FDA‑approved AUD medications.
- Co‑occurring mental‑health support.
- Flexible scheduling or virtual care for tour periods.
Evidence matters more than marketing claims. Amenities are a bonus, not the treatment.
What ‘luxury’ alcohol treatment really changes (and what it doesn’t)
How to get started in Austin (step‑by‑step)
1) Safe withdrawal plan
2) Assessment and schedule
3) Treatment plan anchored in evidence
Expect a mix of counseling, relapse‑prevention skills, and, when appropriate, medication for cravings. Telehealth can bridge gaps while touring.
4) Community and aftercare
Use peer groups (AA, SMART), alumni networks, or sober‑peer channels. Austin’s scene also offers sober activities between sets (parks, lakes, museums), which supports recovery that isn’t centered around nightlife or bar culture.
Break Free from Addiction. Detox Safely in Austin Today.
Medically Supervised Detox – Compassionate Care Starts Here.
How Briarwood Detox Homes Supports Austin Musicians in Outpatient Alcohol & Drug Recovery
Verify Your Insurance Instantly
Don’t guess. Know what’s covered. Click below to verify your insurance coverage with 100% confidentiality and zero obligation.
Medical Disclaimer
Musicians Drug Rehab Locations
Austin Alcohol & Drug Rehab: PAA‑Informed FAQ
What is the difference between inpatient rehab and outpatient rehab?
Inpatient (residential) care provides 24/7 structure and is best when withdrawal risks, safety issues, or triggers are high. Outpatient—especially intensive outpatient programs (IOP)—delivers multiple therapy hours per week while you live at home and keep work or school commitments. Both can be effective; the right fit depends on clinical need and support at home.
How long does outpatient alcohol rehab (IOP) usually take?
Program length varies by assessment and progress, but many IOP plans run several weeks to a few months with step‑downs as you stabilize. Evidence supports IOP as a key part of the continuum when it matches your needs.
When do you need hospital detox for alcohol?
Seek hospital care for severe withdrawal signs such as confusion, hallucinations, seizures, or signs of delirium tremens. These are medical emergencies that require monitored detox and medications.
What happens during hospital alcohol detox?
A team monitors vital signs, treats symptoms, prevents complications, and may use medications to reduce risk and discomfort. Detox is followed by a referral to ongoing treatment like residential, PHP, or outpatient.
Is it safe to detox from alcohol at home?
Not if there’s any chance of moderate to severe withdrawal or a history of complications. Discuss a plan with a clinician; many people need supervised detox to stay safe.
What should I look for in alcohol treatment centers in Austin?
Prioritize evidence‑based care (behavioral therapies plus, when appropriate, FDA‑approved medications for alcohol use disorder), licensed staff, measurement of outcomes, coordination for co‑occurring mental health, and clear aftercare. Use NIAAA’s Navigator to compare programs and ask the right questions.
Does insurance cover alcohol rehab Austin programs?
Coverage varies by plan and level of care. Ask providers to verify benefits and whether they’re in‑network before admission; the NIAAA Navigator lists the key cost and coverage questions to ask.
What levels of care do drug & alcohol rehab Austin providers offer?
Common levels include medical detox, residential/inpatient, partial hospitalization (PHP), intensive outpatient (IOP), standard outpatient, and continuing care. The right level is based on clinical assessment and safety.
Are evening or virtual outpatient groups available in Austin?
Some providers offer evening schedules or telehealth IOP, which can help touring musicians keep work commitments. Confirm availability and licensure for telehealth across any states you travel to.
What is luxury alcohol treatment? Is it more effective?
“Luxury” refers to upgraded amenities (privacy, private rooms, chef‑prepared meals, fitness/spa, scenic settings). Comfort can support engagement, but outcomes are driven by clinical quality—evidence‑based therapies, appropriate medications, and strong aftercare—not amenities alone.
Does music therapy help with addiction?
Evidence suggests music therapy, used alongside standard care, can reduce craving and improve motivation for treatment in some settings; it’s considered an adjunct, not a standalone cure. Results vary across studies and programs.
How do I choose among Austin Texas alcohol rehab options?
Start with a clinical assessment, compare programs using NIAAA’s recommended questions (staff credentials, use of medications, therapy models, outcome tracking), confirm insurance and schedule fit (e.g., IOP evenings), and plan for aftercare.
What happens after rehab?
Good programs build aftercare: relapse‑prevention skills, peer support (AA or secular options), medication management when indicated, and periodic check‑ins. This step helps maintain gains after inpatient or outpatient treatment.
Related Blog Posts
Alcohol Craving Medication During Detox in Austin

Alcohol Detox Austin: How to Detox Safely

Detox Centers in Austin, Texas
Detox Drugs in Austin: What You Should Know
Drug Detox Centers in Austin